Heart transplantation
In the Republic of Belarus, organ transplants are performed in accordance with the law based on the "Presumed consent": an organ may be taken after brain death if the patient have not expressed the wish to the contrary before death.
Recipient
The primary goal of recipient selection is to identify patients with end-stage HF who are unresponsive to medical treatment, but who have the potential to resume a normal active life.
Indications for heart transplantation
Recipients are patients with terminal HF who are not responsive to medication therapy or alternative surgical treatments for heart failure, with the prognosis of one-year survival without transplantation <50%. Objective criteria for this prognosis are: LVEF <20%, serum sodium <135 mEq/L, pulmonary artery occlusion pressure >25 mm Hg, plasma noradrenaline level >600 pg/ml, cardiothoracic index >0.6, reduction of max VO2 <10 ml/kg/min against maximum medication support.
Initial examination of the recipient includes a thorough history analysis and physical examination: chest X-ray, VO2 max test, routine hematological and biochemical tests, serological examination for infectious diseases, determination of human lymphocyte antigen (HLA). Cardiac catheterization with right heart tonometry is mandatory to rule out irreversible pulmonary hypertension before patient is placed on the waiting list for heart transplantation.
Pharmacological bridge to transplantation
Patients with the critical stage of terminal HF require treatment in the intensive care unit with inotropic therapy. In patients with insufficient effect of medication treatment intraaortic balloon counterpulsation is used.
Mechanical bridge to transplantation. In potential recipients who remain hemodynamically unstable for 24–48 hours with maximum pharmacological support, mono-, biventricular, or complete bypass devices are used.
The donor is screened in three stages. The first stage consists of collecting accurate information regarding the patient's age, height, weight, sex, blood type and Rh factor, cause of death, laboratory data, including biochemical tests, and serological tests for infectious diseases (cytomegalovirus, hepatitis B and C). The second stage of screening involves further investigation looking for potential contraindications: ECG, chest radiography, arterial oxygen saturation, and Echo. The final stage of donor screening occurs during organ harvesting surgery: doctors examine ventricular function, valve or coronary pathology.
Donor and recipient compatibility
Compatibility criteria are based on ABO blood type and patient's body size. Donor weight should be within 30% of the recipient's body weight. The recipient is screened for human lymphocyte antigen (HLA) titer. A positive cross-reactivity is an absolute contraindication for transplantation. An increase in the number of panel-reactive antibodies (PRA) of more than 10-15% indicates an increased sensitivity of the recipient to alloantigens.
Our Center uses the classic N. Shumway technique for heart transplantation.
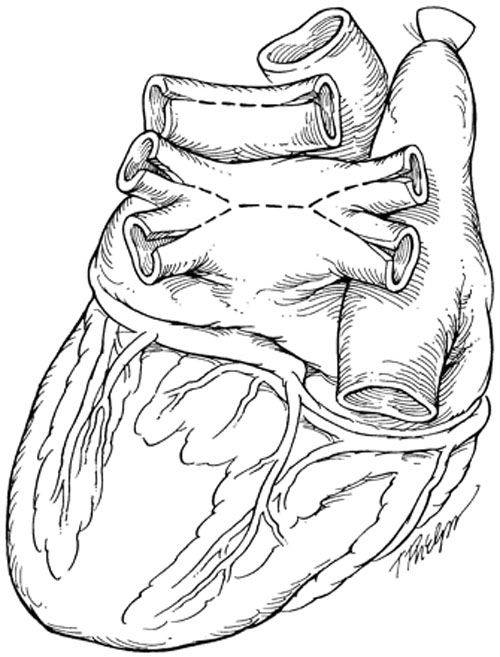 |
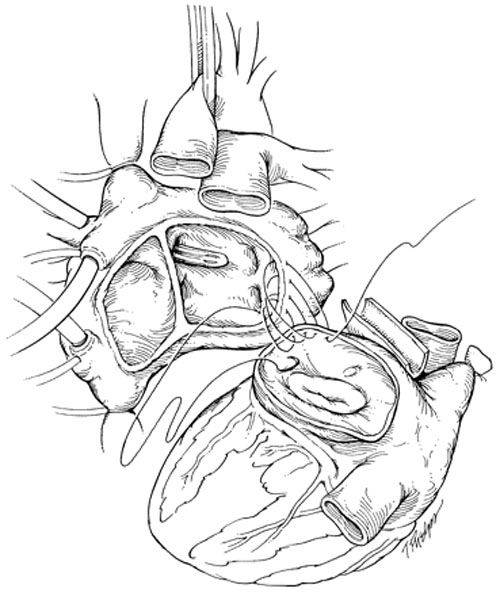 |
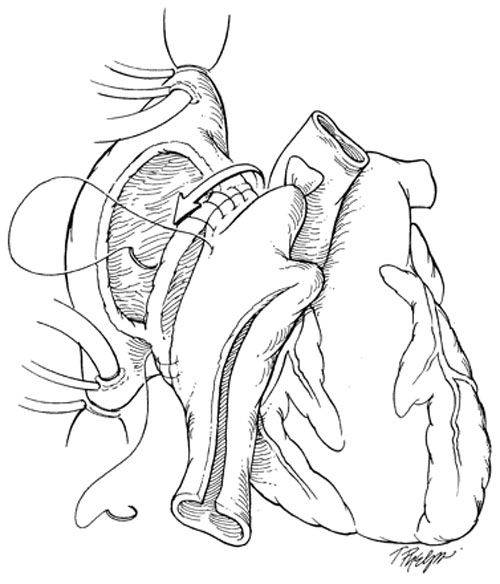 |
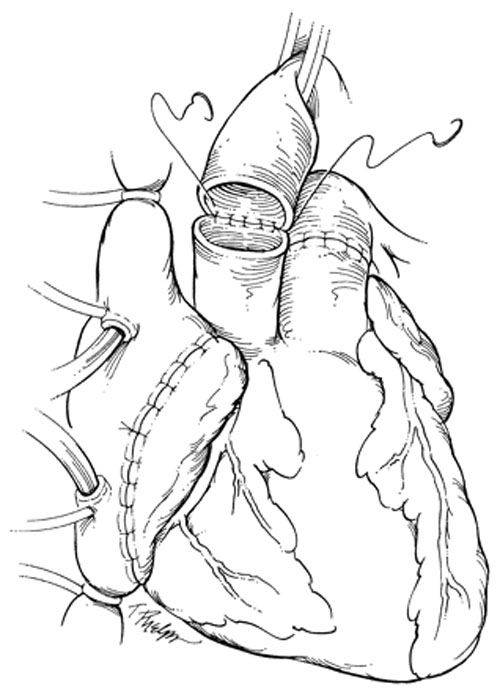 |
Successful and long-term results of orthotopic heart transplantation have made it the method of choice for patients with a lack of effect from medical treatment. However, the obvious limitations of transplantation, including the need for immunosuppression and the shortage of donor organs do not allow this method of treatment to be used in all patients. Alternative surgical methods for HF treatment are widely used in our Center to solve this problem.









